Interview with Brendan Martin by Anna Betz for Enlivening Edge Magazine
Part 2 of this 3-part article is here. Part 3 is here.
Part 1: Shifting mindsets are the seeds to actualizing the next level of health care
Awareness is growing fast that something in the healthcare system needs to change. In fact it is becoming clearer by the day that an absolute rethinking is required in the whole of our healthcare system.
But how can the change that is so absolutely necessary happen when resources necessary for that change are so scarce? A transition to a healthier healthcare system which involves repurposing of resources, re-designation of roles and also the loss of roles can not only be highly disruptive but needs both human as well as financial resources.
Buurtzorg Britain & Ireland, launched in December 2017, is facilitating this transition in the UK and Ireland. Their team supports the growing number of health and social care organisations seeking to apply the lessons from experience of Buurtzorg Nederland, which serves more than 100,000 people through more than 900 self-organised neighbourhood teams in the Netherlands.
According to Brendan Martin, managing director of Buurtzorg Britain and Ireland, the major obstacles in the restructuring process of NHS organizations are mindsets, understandings, and purpose.
He claims that once people really understand the need for restructuring and they have access to resources, they would be able to make the change happen.
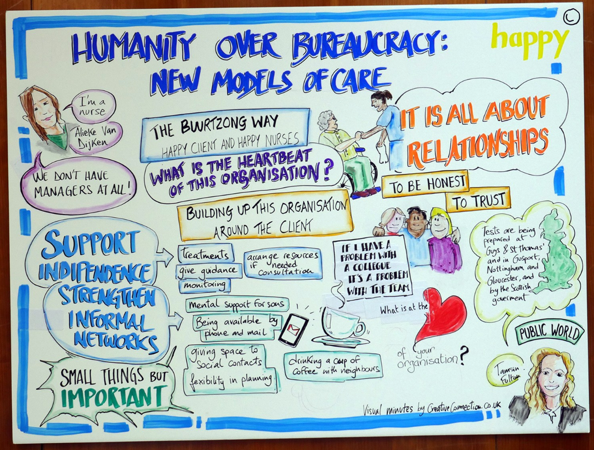
On the positive side, frontline professionals, once they volunteer for the change, are able to learn very quickly. The real and biggest challenge Brendan and his team are encountering in the NHS is with shifting the mindset of organizational leaders, HR , finance (and others who control access to financial resources) and other background services from command and control to true support.
Implementing Buurtzorg principles would mean that some of these background services would no longer be needed and in an organization like the NHS this might not be possible, he believes from his experience so far.
I understand that your team already has some experience in working with various NHS organisation. (See references 1- 4) How do you approach and talk to the NHS and their leaders? How do you open their hearts, minds, and will to listen with curiosity?
We start from where people are, which is a growing awareness that things can’t go on as they are. It is obvious that the NHS and Social Services will just stumble from one crisis to another if they carry on their current trajectory. However, there isn’t a shared understanding about what needs to change.
In engaging with that broader awareness of what needs to change we always go back to first principles as modeled so well by Jos and his fellow founders of Buurtzorg in 2006. It means starting from the perspective of a person needing support.
The Buurtzorg onion model
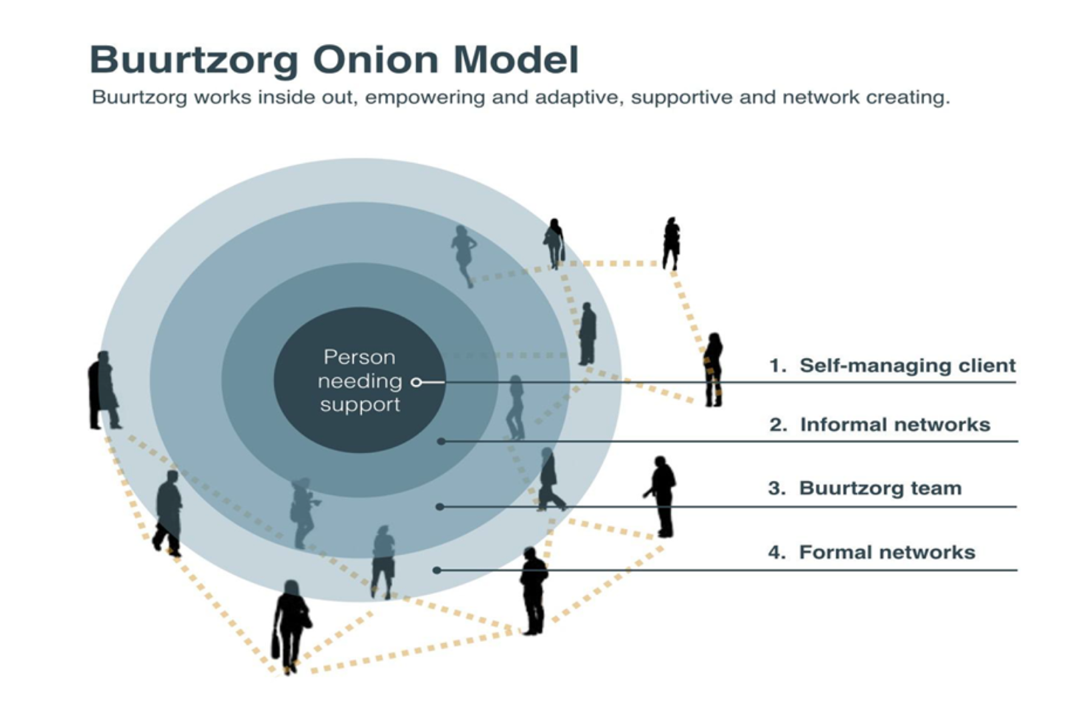
We always start with the Buurtzorg onion model and explain our commitment to that, in both health and social care.
Creating an environment in which professionals are able to provide support, are able to form strong relationships with the person needing support—understanding who they are, where they come from–and pay attention to history, aspirations and dreams—creating that environment is central to the commitment of Buurtzorg UK and Ireland.
Then finding out what the person needing support wants to do, what they can do, and and then working together to mobilize and develop all necessary capacities. Sometimes that involves rekindling capacities and sometimes it means developing new capacities. It means beginning to understand what kind of support can be co-created for the person needing support, and the professional providing it. Also working with the wider social network surrounding the person, family, neighbors depending on location and voluntary organizations is a central aspect of the Buurtzorg model of care.
Supporting clients includes also navigating other parts of the formal system so that support is better coordinated and starts more consistently from peoples’ needs and aspirations.
Building relationships of trust among the caregiver, the cared-for person and the professional and their organizations is fundamental to our work. Trust naturally leads to enabling professionals to exercise the freedom and responsibilities to do their job well, in accordance with vocational commitment and common sense.
The best way for professionals to receive and give support to do their job well is through peers and operating in non–hierarchical small self-organized teams to support and challenge each other to provide and sustain the support needed.
Command and control, the commodification of care work is simply not delivering. It is not only taking humanity away but it is not even succeeding in it own terms, i.e. financial efficiency and effective use of resources. We are actually pushing an open door on that.
Organisational repurposing & cross-sector working to enable the emergence of next stage health care: There are several conversations happening in parallel. Some say you cannot do this in an old organisation and others say that small innovative teams can start this within the existing structure. What is your experience?
Our experience is not yet mature enough to arrive at a firm conclusion. Our approach is to keep working by trying to support organizational change that is needed within existing organizations at the same time to support CICs (Community Interest Companies).
At the fringe, just outside the traditional NHS structure, we are also doing our very best to support the creation of CICs that want to work in the Buurtzorg way and develop an organization influenced by the Buurtzorg experience, supporting them in seeking contracts within the NHS. It is very difficult but not impossible.
We are taking a twin track approach by working both with NHS organisations as well as CICs offering health and care services to the NHS in the UK and Ireland. It is simply too soon to make a definitive judgment about which approach works best.
Within the NHS our longest and most mature test-and-learn projects in South London are nearly eighteen months old. We are at the point where common features manifest themselves and big questions are being asked.
Those pilot projects reach the point now where they show that if their objective is to provide great care, great person-centered and relationship-based care, they clearly do show the way to deliver great care.
If the object is to provide more human jobs and workplace environments, again the experiment shows that that can be done too.
However, none of that is going to gain systemic traction on an organizational level unless you can also show that you can sustain better resource use while reducing cost. The answer to this lies in using both human and material resources in new ways. At the moment that is not happening to the extent required.
Are organizations willing to do what it takes to change and create the organizational conditions for that? Are they prepared to repurpose their organizations, to provide the support that self-organized teams at the front line of care need?
What is needed is an organizational environment in which the people in the back office have a consistent dedication to enabling the front line to enjoy their jobs more and provide great care in a person-centred way and give them the support they need to do that better and better.
Back-office staff and support services need to be prepared to take the same attitude towards their employees as their front line is expected to show towards the people they care for.
This is a big shift from command and control—where you tell staff what to do, and you supervise and discipline them—to your asking staff what they need and then supporting them and working with them to provide it.
Talking about organizational change has big implications how back office functions are organized, for layers of management, for admin functions and how they operate and for whether you need to carry on with some functions at all. Sometimes you just need to stop doing useless things.
At this stage, two years into what we have been trying to do in the NHS, this is the big question that remains unanswered.
References
1.Hounslow Community Learning Disability Team at Hounslow and Richmond Community Healthcare NHS Trust
2. Evaluating the application of the Buurtzorg principles in Scotland
Evaluating the application of the Buurtzorg principles in Scotland
3. The Guy’s and St Thomas’ NHS Foundation Trust Neighbourhood Nursing Team Test and Learn project of an adapted Buurtzorg model: An early view
London trust to roll out Buurtzorg community nursing model 16 JANUARY, 2018
4. West Suffolk Briefing
Blog posts published by East of England Local Government Association (Eelga)
- January 2018 – Tackling staffing shortages in health and social care
- October 2017 – Creating a culture of self-management
- July 2017 – Recruiting a self-managing team
- June 2017 – West Suffolk Test and Learn recruits it first nurses!
- May 2017 – Buurtzorg inspired project features on BBC Look East
- March 2017 – Buurtzorg inspired Test and Learn in West Suffolk is given the go ahead
- November 2016 – Partners see Buurtzorg in action
- October 2016 – Examining the Buurtzorg Model First Hand
- June 2016 – West Suffolk Gets a Visit from a Buurtzorg Nurse: Meet Madelon Van Tilburg
 Brendan Martin is founder and Managing Director of Public World and Buurtzorg Britain & Ireland, which work to support better care and services and more fun at work through self-managed teams in high trust organisations. www.buurtzorg.org.uk
Brendan Martin is founder and Managing Director of Public World and Buurtzorg Britain & Ireland, which work to support better care and services and more fun at work through self-managed teams in high trust organisations. www.buurtzorg.org.uk
 Anna’s background is in Health and Social Care with training in Herbal Medicine, Socialwork, Mindfulness Practice, Transparent Communication, and Systemic Family Therapy. She practices a pro-active evolutionary approach to Health and Wellbeing and leads on projects in the UK National Health Service using Mindfulness and diet for people suffering from chronic inflammatory diseases like diabetes and dementia. Her passion for building thriving and sustainable communities inspired her to co-found the HealthCommonsHub. She feels at home in places where individual, communal, organisational, and social evolution meet, and where people support each other in becoming whole and feel enlivened.
Anna’s background is in Health and Social Care with training in Herbal Medicine, Socialwork, Mindfulness Practice, Transparent Communication, and Systemic Family Therapy. She practices a pro-active evolutionary approach to Health and Wellbeing and leads on projects in the UK National Health Service using Mindfulness and diet for people suffering from chronic inflammatory diseases like diabetes and dementia. Her passion for building thriving and sustainable communities inspired her to co-found the HealthCommonsHub. She feels at home in places where individual, communal, organisational, and social evolution meet, and where people support each other in becoming whole and feel enlivened.




Here in the you can find feedback from patients and carers about the new Neighbourhood Nursing teams :
The Guy’s and St Thomas’ NHS Foundation Trust Neighbourhood Nursing Team Test and Learn project of an adapted Buurtzorg model: An early view
By Vari M Drennan MBE, Fiona Ross CBE, Mary Saunders and Peter West. December 2017
Source: p.11/51
http://eprints.kingston.ac.uk/40416/1/The%20Guy%E2%80%99s%20and%20St%20Thomas%E2%80%99%20NHS%20Foundation%20Trust%20Neighbourhood%20Nursing%20Team%20an%20early%20view%20evaluation%20report%20%202017%20FINAL%20WEB%20VERSION%20December.pdf
Carer’s feedback: ” I think neighbourhood nurses are the best solution so far to trying to keep people monitored who are not in hospital that have got conditions and giving them the support they need to keep them out of hospital.”
Patient feedback: “I was very pleased with the care I received. They were unhurried and quite informative … I would thoroughly recommend them to anybody in my situation.,”